Weak bones are bad news. Osteoporosis, the most severe form of weak bones, carries an increased risk of fracture. If you fracture your hip you will very likely lose your independence and shorten your life. The mortality rate following a hip fracture is 27% within 1 year and 79% by 4 years.(1) Yikes–that’s not good!
The diagnosis of osteoporosis is made by a dexa scan. This is an x-ray study of the bones, where a computer program estimates the density of the bones based on their appearance. Osteopenia is another possible diagnosis, which means that your bones are clearly less-dense than normal, but not bad enough to meet the criteria for osteoporosis.
Neither of these diagnoses are good, and if you’ve received one of them you’ve probably been offered medication to increase bone density. These medications definitely do increase bone density. But do they really make the bones stronger, or just LOOK better on x-ray? The medications also have potential bad side effects, like esophageal ulcers, jaw necrosis, and atypical fractures after prolonged use.(2-5) Could there be a better way to get strong bones?
What is bone strength?
First let’s talk about the ultimate goal. What do you really want? An active, independent, long life, right? No fractures that limit mobility, rob our independence, and increase our risk of death. We need strong bones.
Bone strength is a combination of bone density and bone quality–read that again! You need BOTH density and quality to have strong bones. Unfortunately, a dexa scan does not measure bone quality–it only measures density. Think of an oak tree. It may look really strong, but if it’s not flexible it will snap in a windstorm. Dense and brittle is not helpful.
This topic is near and dear to me. As a gynecologist for over 2 decades, I used to regularly prescribe medication to women to improve their bone density. I thought I was helping them.
But then I learned of this thing called a “black box warning.” It declared that after 5 years many of these medications increased the risk of “atypical fractures”. WHAT? I thought I was helping prevent fractures, not increasing the risk of a weird type of fracture caused by minimal trauma!
Oh, and how can something be helpful for 4 years and 11 months, and then at 5 years be bad? That just didn’t make sense to me! I wanted to help women live quality lives, without “black box warnings”. This was actually one of my “aha moments” that drove me to look at health from a more holistic perspective, and I’m so glad I did!
7 tips for strong bones–NATURALLY
We want to make your bones STRONGER, not just more dense. And without nasty potential side effects. Here are my top 7 tips to naturally increase bone strength:
1. Eat enough protein
Protein actually forms the scaffolding to which the minerals attach. Picture this– the strength of a wall is the strength of your bones. What you SEE on the wall is the drywall, but the strength of the wall is from the studs. Protein is the studs in your bone-wall. Many people do not get enough protein in their diet and therefore don’t have enough studs in their bone-walls to provide adequate strength.
How much protein is enough? A good estimate is 0.36 grams of protein per pound body weight. So if you weigh 150 pounds you should be getting AT LEAST 54 grams of protein daily. This translates to about 8 ounces of meat, fish, or poultry, or 8 eggs. That’s because 1 ounce of meat or 1 egg contains about 7 grams of protein. Notice that I said “at least”. “Minimum” means you can have more than that but not less. Please note that this does NOT apply to you if you have kidney disease… If you have kidney disease you might need to be on a protein-restricted diet. Please talk to your physician.
2. Exercise
Putting it simply, strong muscles equal strong bones. You can strengthen your muscles with weight-bearing exercise and resistance training (lifting weights). Weight-bearing exercise includes:
- Walking
- Climbing stairs
- Dancing
- Jogging
Proper weight training puts just the right amount of tension on your bones to stimulate growth and strength. Concentrate primarily on your core, which is the area from your belly button to your knees. This will increase hip-bone strength to prevent life-altering hip fractures.
Proper weight training also implies adequate rest between exercises, otherwise you are overtraining. Overtraining causes muscle breakdown rather than building, and that’s not good! The recommended amount of rest needed between exercising the same muscle group is 48-72 hours. And for women over 50, I recommend 72 hours.
The benefit of exercise actually happens BETWEEN the exercise days. THAT’S when your body rebuilds stronger. If you exercise the same groups before the repair is complete, then you are just breaking things down. That’s why overtraining is BAD.
3. Optimize your micronutrients
Micronutrients are like tools in the toolbox, helping the body get the job done–in this case maintaining strong bones. I’d like to address several key micronutrients, as well as a few out-dated ideas:
- Calcium
- Vitamin K2
- Vitamin D
- Magnesium
- Boron
- Strontium
Calcium is what everyone thinks of as the key component to bone health
Calcium is the mineral with the highest concentration in bone. There is a bit of controversy about the amount of dietary calcium needed to maintain healthy bones. The range is from 600-1200 mg for adults, depending on who you ask.(6-7) One thing that most agree on is that dietary sources of calcium are better absorbed than supplements. Dietary sources of calcium include:
- Canned, bone-in fish (sardines, salmon, anchovies)
- Dark-green leafy vegetables
- Seeds (especially poppy and sesame)
- Almonds
- Dairy (but this is not a preferred source because a lot of people are sensitive to dairy)
However, the concept that bone loss is from not enough calcium is a myth. Bone loss is actually a mismanagement of calcium. Let me explain! Inappropriate aging results in calcium leaving your bones and depositing in your bones and arteries–yikes! Simply taking more calcium won’t help if it doesn’t go to the right place.
Enter Vitamin K2.
This important vitamin helps to ensure proper calcium management–keep it in the bones and avoid the arteries and joints!(8) The official Recommended Dietary Allowance (RDA) of vitamin K is not that helpful relating to bone health, as it is based solely on vitamin K1 and blood clotting. It has not been updated to include bone strength. There are studies looking at vitamin K2 (MK4 and MK7) and bone health, and the range studied was 50-180 micrograms.(9-10)
Vitamin K2 isn’t easily available from food sources, other than natto (fermented soy). If you take a supplement, make sure to read the label specifically for whether K1 or K2 is the form, as only vitamin K2 has been shown to improve bone strength.
Vitamin D is very important for bone health!
Vitamin D:
- Is essential for calcium absorption.
- Helps with the deposition of calcium onto the protein scaffolding, increasing bone density.
- Improves muscle-building, thus increasing a powerful stimulus to build stronger bones.(11)
Optimizing Vitamin D requires either sun exposure or supplementation, as it’s not available in high quantities from food. Your skin makes Vitamin D out of cholesterol, when triggered by ultraviolet light from sun exposure. People living in northern latitudes are more likely to need a supplement, because the angle of the sun on the earth at these latitudes does not trigger the response.
If you take vitamin D, know that it’s a fat-soluble vitamin, which means levels will accumulate over time. You can check your level by measuring a serum 25-hydrox-vitamin D level (25-OHD). The reference range at most labs is 30-100 ng/ml. The Vitamin D Council recommends a level of 40-60 ng/ml for bone health.(12) I actually prefer a level of 60-80, in order to get the added-benefit of immune-system support.
Magnesium plays multiple roles in maintaining bone health…
Magnesium is:
- Part of the mineral content of bone
- Necessary for vitamin D synthesis
- Anti-inflammatory
Unfortunately many people are deficient in magnesium. Low magnesium is associated with an increased fracture risk.(13) The RDA for magnesium ranges from 310-420 mg elemental magnesium, depending on gender and age.(14)
Dietary sources of magnesium include:
- Legumes
- Leafy vegetables
- Nuts
- Whole grains
Here’s the thing though… Plants can only give YOU magnesium, if THEY can get it from the soil. And with the years of industrial farming, the soil is very low in magnesium. It’s not one of the big-3 (N-P-K=nitrogen, phosphorus, potassium) that make it into most fertilizers.
Most of my clients need to supplement with magnesium. When choosing a supplement, make sure that you get information on how much ELEMENTAL magnesium it contains, not just the weight of the entire complex. Magnesium comes as a salt, and the component that it is attached to affects how much elemental magnesium is in each capsule. My favorite forms of magnesium are:
- Magnesium Citrate–helps loosen your stool, so it’s great if you struggle with constipation
- Magnesium Malate–displaces lactic acid, so it’s great if you have sore muscles
- Magnesium Threonate–crosses the blood-brain barrier and helps with relaxation
Boron plays a back-stage role in bone health..
This is by its effect on magnesium and calcium. Boron deficiency leads to too much calcium excretion and not enough magnesium absorption. The recommended “safe levels” of boron vary widely, from 1-13 mg. (15-16)
The following foods are good sources of boron:
- Almonds
- Apricots
- Avocados
- Cashews
- Dates
- Hazelnuts
- Lentils
Strontium used to be considered good for bones, but this idea is outdated.
Strontium is BAD for bones, because it displaces magnesium and calcium in your bones. In effect, it makes your bones LOOK more dense, but NOT function better.(17) Did you know that Lead also will make your bones look more dense, because it is stored in your bones at the expense of calcium and magnesium? It’s time to take strontium OUT of the recommendations for bone health.
4. Reduce inflammation
Inflammation is a problem, because it causes acidity, and acid eats bone.(18) PERIOD! C-Reactive Protein (CRP) is a marker of inflammation, and elevated CRP is associated with osteoporosis.(19) Chemicals called cytokines are released from the immune system during inflammation, increasing bone breakdown.
Lifestyle factors play a key role in inflammation. Two strategies to decrease inflammation are to decrease things that cause inflammation, and increase things that reduce inflammation. Here are specific things you can do to reduce inflammation (20-21):
- Avoid added sugar in your diet
- Reduce your intake of processed foods
- Don’t drink excessive alcohol
- Don’t smoke cigarettes
- Increase vegetables in your diet
- Increase fiber in your diet
- Increase omega-3 fatty acids
- Exercise but don’t over-train
- Increase antioxidant intake of vitamins C, E and A
5. Improve gut health
Intestinal health is crucial for several reasons:
- We have to be able to absorb the raw materials, protein and minerals, to make healthy bones.
- An unhealthy gut leads to inflammation, which is bad for bones, as I discussed above.
How do you know if you have an unhealthy gut? Well, if you are constantly aware of your gut, ie it is talking to you all day via bloating, gas, gurgling, discomfort, it’s not healthy! Another sign is constipation or diarrhea. A healthy gut is our silent partner, quietly doing its job of absorbing nutrients and excreting waste without making a lot of noise. Exactly HOW to improve gut health is beyond the scope of this article, as I could write a whole book about it! Just know that it’s important and seek help if you have issues.
6. Optimize hormones that impact bone health
Many hormones impact bone health. I want to discuss these:
- Testosterone
- Estrogen
- Cortisol
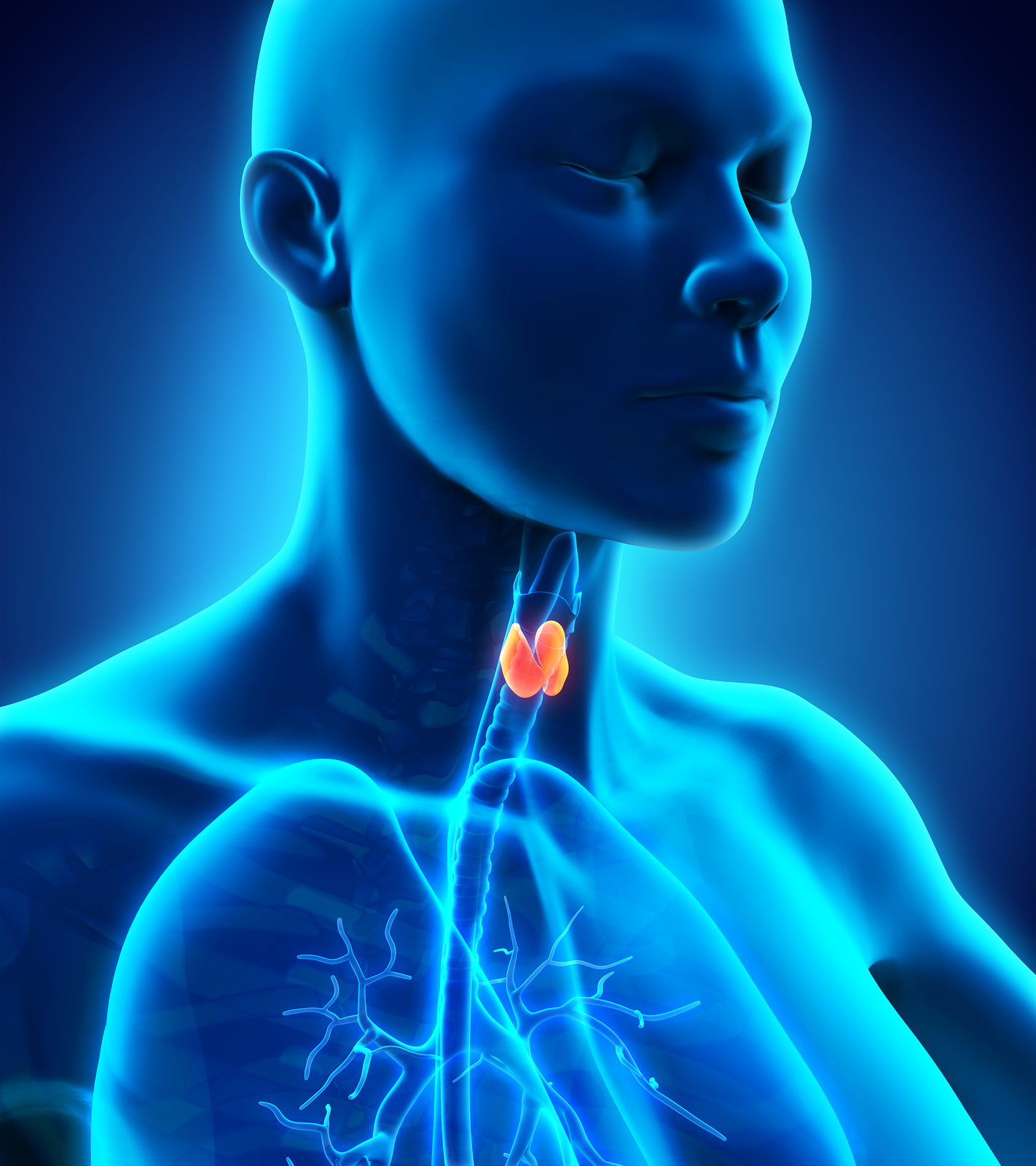
- Thyroid
- Insulin
Testosterone and Estrogen
These sex-steroids are good for bones.(22) Almost all women in menopause have low estrogen, unless they are on hormone replacement, and many also have low testosterone. Not a lot of doctors offer testosterone testing to women. Moreover, many lab companies go almost to ZERO when defining the normal range for free testosterone levels in women. If you are interested in learning more about hormone-replacement therapy follow this link to a separate post on the topic.
Cortisol is BAD for bones!
Cortisol is your stress hormone. High stress leads to high cortisol, and prolonged high cortisol eats you up like acid from the inside out.(23-25)
When it comes to stress we seem to have blinders on. We’d all agree that a life-threatening emergency is stressful, but so is a to-do list that is too long. And unfortunately our society wears “busyness” like a frickin badge of honor!
Your body only has one response to stress and that’s cortisol. We NEED to step out of the rat-race and calm down. Now, I understand that there are things we CAN’T control, like the decisions our newly-adult children make, our aging parents, our spouse’s health… But we CAN make time to sit quietly and activate our relaxation mode–the parasympathetic nervous system.
Lots of options for promoting relaxation:
- Guided meditations (link here for more on this topic)
- Gratitude journal
- Tapping/acupressure
- Neurofeedback (link here for more information on this therapy)
- Acupuncture
Thyroid hormone is a “Goldy-Locks” hormone when it comes to bones.
You NEED thyroid hormone to make energy, and it takes energy to keep your bones strong… but it can affect bone health negatively, IF you have too much. Hyperthyroidism is associated with accelerated bone loss. However, in my opinion (and that of many functional-medicine doctors), the diagnosis of hyperthyroidism should be based on measuring the free thyroid hormones (Free T3 and Free T4) and not just thyroid stimulating hormone (TSH). That’s because TSH is NOT thyroid hormone. It’s a stimulating hormone made in the brain to trigger thyroid hormone production when the body needs it.
High insulin is bad for bones.
Chronic high insulin increases inflammation, and inflammation eats your bones like acid (sorry if I sound like a broken record here, but I truly believe that inflammation is the root of almost ALL our health problems!) Methods of lowering insulin naturally include avoiding high-sugar-and-starch foods and intermittent fasting.
7. Get the RIGHT amount of sleep
Sleep is another “Goldy-Locks” variable regarding bone health. Multiple studies show a relationship between too little or too much sleep and osteoporosis.(26-27)
My take on “too much sleep” is because it’s part of being sedentary. Too much sleep implies that you aren’t being active enough and THAT is bad for bones.The ideal amount of sleep for optimal bone health is 8-9 hours a night. Significantly less or more than that can have a negative impact on bone health.
Most of us, however, don’t get enough sleep, and that is BAD! Sleep is when your body repairs. Growth hormone is released during sleep, and this is a very important hormone for repair, as well as muscle and bone health.(28) Poor sleep is also associated with increased inflammation, and that leads to increased bone loss (same song 3rd verse…).
If you struggle with sleep try these things:
- Keep a consistent sleep schedule, going to bed and getting up at a similar time
- Sleep in a dark, cool room
- Avoid caffeine within 8 hours of bed time
- Don’t eat within 3 hours of bed time
- Don’t nap past 3 pm
- Get at least 30 minutes of natural sunlight daily, preferably first thing in the morning
- Do something relaxing for the 2-hours preceding bed time
- Avoid computer screens within 2 hours of bed time
- Turn your wifi off at night
If you still struggle with sleep after doing these things, make sure to see a doctor. Sleep is very important for your bone (and general) health.
Wrapping it up
So you see? There’s A LOT we can do to improve bone health WITHOUT taking risky medications! The beauty of the above tips is that they will improve many other aspects of your health, in addition to strengthening your bones. So everybody wins! You don’t have to WAIT until you have a diagnosis of osteopenia to start strengthening your bones. Because these suggestions are not risky, and help other aspects of your health, why not start right now?
If you DO have a diagnosis of osteopenia or osteoporosis then you need to start, like YESTERDAY! Make sure you are working with someone that understands the nuances of hormones and micronutrients. You don’t want to be on the 4-years-and-11-months plan of “good for you” until it’s not, like some of the medications. Risk aside, if something can be achieved without medication, shouldn’t that be the superior way anyway?
References
-
Panula J, Pihlajamäki H, Mattila VM, Jaatinen P, Vahlberg T, Aarnio P, Kivelä SL. Mortality and cause of death in hip fracture patients aged 65 or older: a population-based study. BMC Musculoskelet Disord. 2011 May 20;12:105. doi: 10.1186/1471-2474-12-105. PMID: 21599967; PMCID: PMC3118151.
-
Green, J. (2010, June 23). Oral bisphosphonates and risk of cancer of esophagus, stomach, and colorectum: case-control analysis within a UK primary care cohort. Retrieved from https://www.bmj.com/content/341/bmj.c4444
-
Ruggerio, S. et al. (2014 October). American Association of Oral and Maxillofacial Surgeons Position Paper on Medication-Related Osteonecrosis of the Jaw—2014 Update. Journal of Oral Maxillofacial Surgery. Retrieved from https://www.joms.org/article/S0278-2391%2814%2900463-7/abstract
-
Prasarn, M.L. et al. (2012, June 6). Bisphosphonate-associated Femur Fractures Have High Complication Rates with Operative Fixation. Clinical Orthopaedics and Related Research. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3392377/#CR1
-
https://www.accessdata.fda.gov/drugsatfda_docs/label/2021/125320s207lbl.pdf
-
https://ods.od.nih.gov/factsheets/Calcium-HealthProfessional/
-
Michaëlsson K, Melhus H, Warensjö Lemming E, Wolk A, Byberg L. Long term calcium intake and rates of all cause and cardiovascular mortality: community based prospective longitudinal cohort study BMJ 2013; 346 :f228 doi:10.1136/bmj.f228
-
McCabe KM, Booth SL, Fu X, Shobeiri N, Pang JJ, Adams MA, Holden RM. Dietary vitamin K and therapeutic warfarin alter the susceptibility to vascular calcification in experimental chronic kidney disease. Kidney Int. 2013 May;83(5):835-44. doi: 10.1038/ki.2012.477. Epub 2013 Jan 23. PMID: 23344475.
-
Inaba N., Sato T., Yamashita T. Low-dose daily intake of vitamin K2 (Menaquinone-7) improves osteocalcin γ-carboxylation: A double-blind, randomized controlled trial. J. Nutr. Sci. Vitaminol. 2015;61:471–480. doi: 10.3177/jnsv.61.471.
-
Knapen M.H., Drummen N.E., Smit E., Vermeer C., Theuwissen E. Three-year low-dose menaquinone-7 supplementation helps decrease bone loss in healthy postmenopausal women. Osteoporos Int. 2013;24:2499–2507. doi: 10.1007/s00198-013-2325-6.
-
Laird E, Ward M, McSorley E, Strain JJ, Wallace J. Vitamin D and bone health: potential mechanisms. Nutrients. 2010 Jul;2(7):693-724. doi: 10.3390/nu2070693. Epub 2010 Jul 5. PMID: 22254049; PMCID: PMC3257679.
-
https://www.vitamindcouncil.org/
-
Kunutsor SK, Whitehouse MR, Blom AW, Laukkanen JA. Low serum magnesium levels are associated with increased risk of fractures: a long-term prospective cohort study. Eur J Epidemiol. 2017;32:593–603. doi: 10.1007/s10654-017-0242-2.
-
https://ods.od.nih.gov/factsheets/magnesium-healthprofessional/
-
https://pubmed.ncbi.nlm.nih.gov/7889887/
-
https://ods.od.nih.gov/factsheets/Boron-HealthProfessional/
-
https://www.ema.europa.eu/en/news/prac-recommends-suspending-use-protelososseor
-
Ginaldi, L., Di Benedetto, M.C. & De Martinis, M. Osteoporosis, inflammation and ageing. Immun Ageing 2, 14 (2005). https://doi.org/10.1186/1742-4933-2-14
-
Ganesan K, Teklehaimanot S, Tran TH, Asuncion M, Norris K: Relationship of C-reactive protein and bone mineral density in community-dwelling elderly females. J Natl Med Assoc. 2005, 97: 329-33.
-
Kantor ED, Lampe JW, Kratz M, White E. Lifestyle factors and inflammation: associations by body mass index. PLoS One. 2013 Jul 2;8(7):e67833. doi: 10.1371/journal.pone.0067833. PMID: 23844105; PMCID: PMC3699492.
-
Jarvandi S, Davidson NO, Jeffe DB, Schootman M. Influence of lifestyle factors on inflammation in men and women with type 2 diabetes: results from the National Health and Nutrition Examination Survey, 1999-2004. Ann Behav Med. 2012 Dec;44(3):399-407. doi: 10.1007/s12160-012-9397-y. PMID: 22865468; PMCID: PMC3590805
-
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5539371/
-
Follis SL, Bea J, Klimentidis Y, Hu C, Crandall CJ, Garcia DO, Shadyab AH, Nassir R, Chen Z. Psychosocial stress and bone loss among postmenopausal women: results from the Women’s Health Initiative. J Epidemiol Community Health. 2019 Sep;73(9):888-892. doi: 10.1136/jech-2019-212516. Epub 2019 Jul 9. PMID: 31289118.
-
Pahk K, Kwon HW, Joung C, Kim S. Stress-Related Amygdala Metabolic Activity Is Associated With Low Bone Mineral Density in Postmenopausal Women: A Pilot 18F-FDG PET/CT Study. Front Endocrinol (Lausanne). 2021 Aug 12;12:719265. doi: 10.3389/fendo.2021.719265. PMID: 34475851; PMCID: PMC8406934.
-
Mitra R. Adverse effects of corticosteroids on bone metabolism: a review. PM R. 2011 May;3(5):466-71; quiz 471. doi: 10.1016/j.pmrj.2011.02.017. PMID: 21570035
-
Fu, X., X. Zhao, H. Lu, F. Jiang, X. Ma, and S. Zhu. 2011. Association between sleep duration and bone mineral density in Chinese women. Bone 49(5):1062–1066.
-
Chen G, Chen L, Wen J, Yao J, Li L, Lin L, Tang K, Huang H, Liang J, Lin W, Chen H, Li M, Gong X, Peng S, Lu J, Bi Y, Ning G. Associations between sleep duration, daytime nap duration, and osteoporosis vary by sex, menopause, and sleep quality. J Clin Endocrinol Metab. 2014 Aug;99(8):2869-77. doi: 10.1210/jc.2013-3629. Epub 2014 May 21. PMID: 24848706.
-
https://www.nhlbi.nih.gov/resources/brief-your-guide-healthy-sleep